Our emergency trauma team spots shock in ER when symptoms are still subtle. We start treatment right away with fluids and medication, often before patients realize how serious their condition has become.
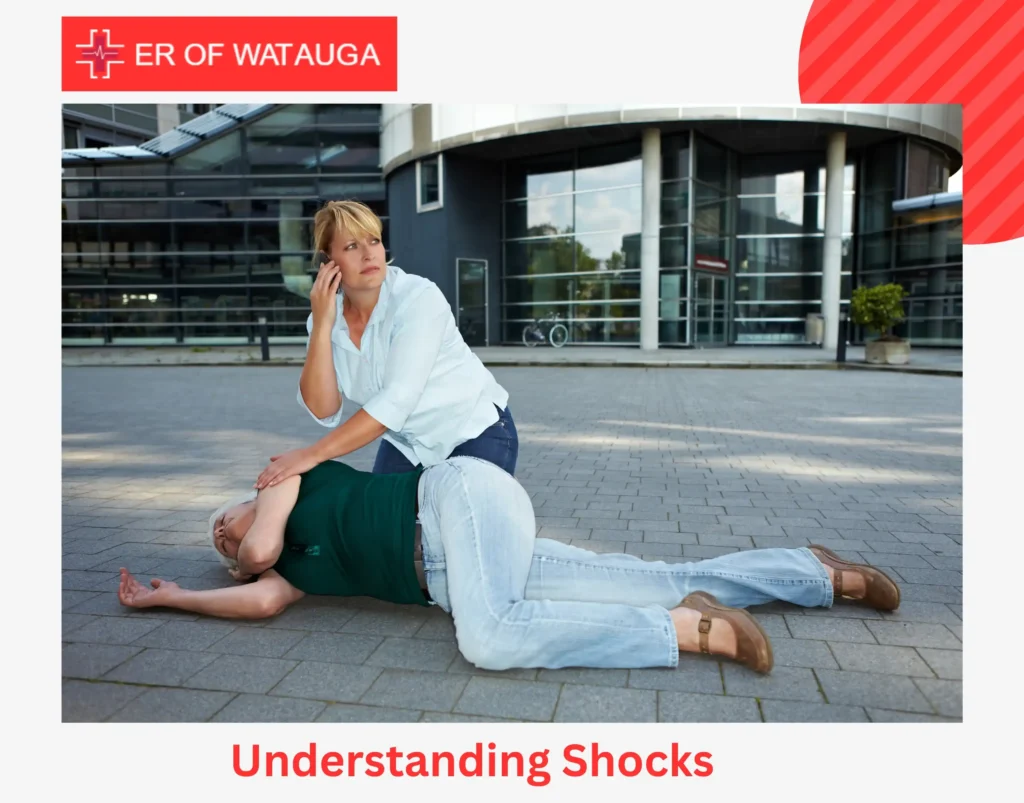
Understanding Shocks
Shock is a critical medical state that can result from various causes, including severe blood loss, infections, heart conditions, or trauma. When the circulatory system fails to deliver enough oxygen and nutrients to vital organs, the body begins to shut down, posing severe health risks. Shock is classified into different types, each with distinct causes and symptoms.
Types of Shocks
- Hypovolemic Shock – Happens when the body loses a critical amount of blood or fluids due to serious injuries, burns, or dehydration. This leads to dangerously low blood volume, hindering circulation and oxygen delivery.
- Cardiogenic Shock – Arises when the heart cannot pump adequate blood, often triggered by a heart attack, severe arrhythmia, or cardiac arrest. If there is no intervention, this can result in multiple organ failures.
- Septic Shock – A life threatening reaction to severe infections, leading to widespread inflammation and a dramatic decrease in blood pressure. This condition can swiftly harm tissues and organs if not treated with vigorous medical intervention.
- Anaphylactic Shock – A severe allergic response that causes swelling of the airways, issues with breathing, and a sudden drop in blood pressure. Without immediate administration of epinephrine, it can become life-threatening within minutes.
- Neurogenic Shock – Occurs as a result of spinal cord injuries that disrupt the nervous system’s control over blood vessel constriction, resulting in sudden dilation, reduced circulation, and extremely low blood pressure.
Emergency Shock Symptoms
Identifying the emergency shock symptoms early can be life-saving. As the body struggles to maintain circulation and oxygen delivery, a series of distress signals emerge. Here’s what to watch for:
Altered Mental State
Reduced blood flow to the brain can cause confusion, agitation, and restlessness. In severe cases, disorientation worsens, leading to unconsciousness, requiring immediate intervention in the ER.
Abnormal Heart Rate and Weak Pulse
The heart may initially beat rapidly to compensate for oxygen loss, but as shock progresses, the pulse can become weak or irregular, signaling a critical need for emergency care.
Cold, Clammy Skin and Discoloration
Blood is redirected to vital organs, leaving the skin pale, sweaty, and cool. A bluish tint on the lips or extremities indicates severe oxygen deprivation, a serious concern in shock cases treated in the ER.
Rapid, Shallow Breathing
The body increases respiratory rate to compensate for low oxygen levels. In an ER setting, oxygen support or ventilation may be necessary to stabilize breathing.
Severely Low Blood Pressure
A key indicator of shock, dangerously low blood pressure can cause dizziness, fainting, and organ failure. In the ER, IV fluids and medications are used to restore circulation.
Drastically Reduced Urine Output
The kidneys struggle due to inadequate blood flow, resulting in little to no urine production, a critical warning sign requiring immediate medical intervention.
Digestive System Distress
Nausea, vomiting, and abdominal discomfort occur as the body prioritizes vital organs. ER teams monitor these symptoms closely while treating the underlying cause of shock.
Early identification of shock in ER is critical for effective treatment and improved outcomes. Emergency responders quickly assess vital signs, administer IV fluids, oxygen, or life-saving medications to prevent irreversible damage and improve survival chances.
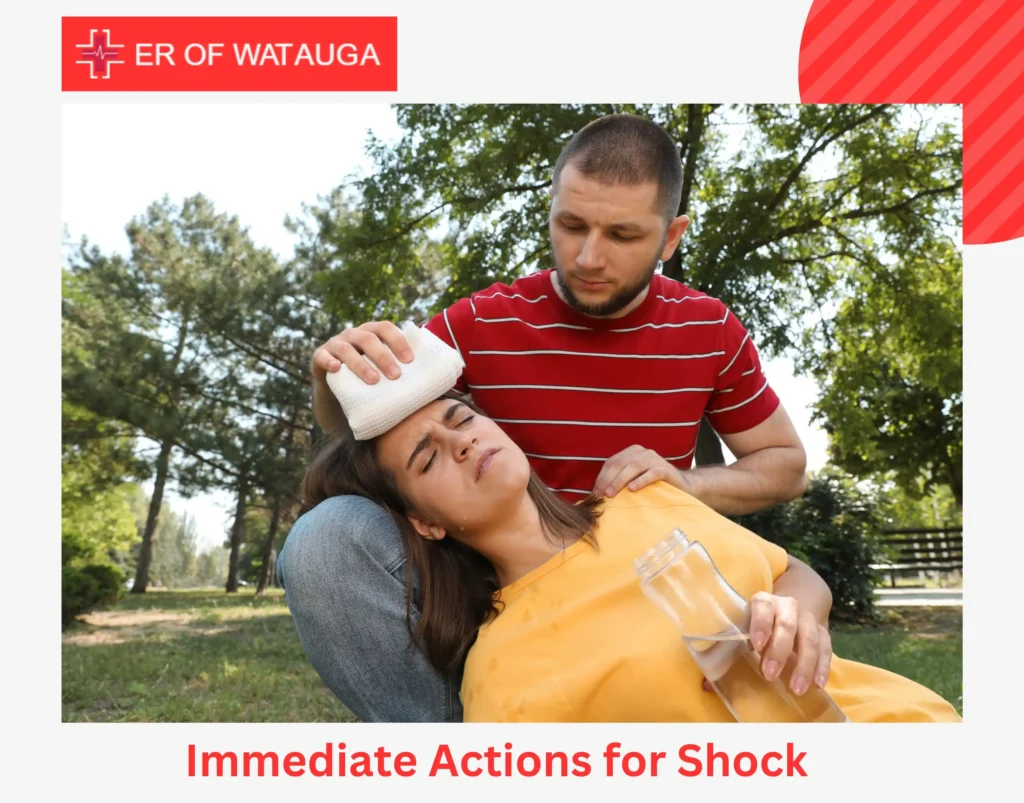
Immediate Actions for Shock
When signs of shock appear, quick medical intervention is crucial. Here’s how to respond:
Call 911 Immediately
Shock is a medical emergency that requires professional treatment.
Lay the Person Down
Elevate the legs (unless there is a spinal, head, or leg injury) to improve blood flow to the brain and heart.
Keep the Person Warm
Use blankets or clothing to maintain body temperature and prevent hypothermia.
Monitor Breathing and Pulse
If the person stops breathing, begin CPR if trained to do so.
Do Not Give Food or Drinks
Shock impairs digestion, and fluids could cause choking.
Treatment of Shock in ER
In the emergency room, medical professionals quickly evaluate and stabilize patients using:
Oxygen Therapy
- Additional oxygen enhances circulation and aids essential organ function.
Intravenous Fluids & Blood Transfusion
- IV fluids assist in restoring blood volume, particularly in instances of hypovolemic shock.
- Blood transfusions might be necessary for considerable blood loss.
Medications
- Vasopressors: Narrow blood vessels to increase blood pressure
- Antibiotics: Fight infections in cases of septic shock
- Epinephrine: Neutralizes severe allergic responses in anaphylactic shock
Surgical & Procedural Interventions
- Cardiogenic shock: May need cardiac procedures such as angioplasty
- Neurogenic shock: Surgery may be required to stabilize the spine
Long-Term Health Risks of Shock in ER
Even after successful treatment, shock in ER cases can lead to serious health risks:
- Organ Injury – Extended oxygen deprivation may lead to lasting harm to the kidneys, liver, or brain.
- Heart Issues – Cardiogenic shock heightens the risk of future heart failure.
- Neurological Problems – Neurogenic shock can lead to permanent impairment of the nervous system.
- Increased Infection Risk – Those who survive septic shock are more susceptible to recurring infections.
Preventing Shock
While not all types of shock are preventable, taking precautions can reduce the risk:
- Control Chronic Conditions – Proper management of heart disease, diabetes, and infections can help avoid complications.
- Identify Emergency Shock Symptoms – Quick recognition of emergency shock symptoms enables faster medical response.
- Stay Hydrated – Avoid severe dehydration, particularly in hot or dry environments.
- Be Prepared for Allergies – Keep an epinephrine auto-injector on hand if you are susceptible to severe allergic reactions.
- Prioritize Safety – Use seat belts, helmets, and protective gear to lower the risk of trauma-related shock in ER
Key Takeaway
Certain symptoms should never be ignored, especially when they indicate shock in ER cases. Signs such as rapid heartbeat, shallow breathing, cold or clammy skin, confusion, and a weak pulse require immediate medical attention.
Recognizing emergency shock symptoms early and seeking prompt care can improve recovery and reduce health risks. If you’re ever unsure about the severity of your condition, it’s always safer to consult a medical professional.
At Watauga ER, our expert team provides 24/7 emergency care for shock and other life-threatening conditions. We ensure immediate evaluation and treatment, helping you get the care you need without delays.
FAQs
What is the difference between fainting and shock?
Fainting is a brief loss of consciousness due to low blood pressure, while shock is a life threatening condition with inadequate blood flow to vital organs.
What is the priority in treating shock?
The priority is to restore blood flow and oxygen to vital organs by ensuring the person is kept warm, lying down, and receiving immediate medical treatment.